The U.S. healthcare market is undergoing a lot of changes; it is redefining the industry and altering the way it’s associated organizations do business.
The result is essentially a new model for the nation’s healthcare system. It’s a “perfect storm” with care and cost at its centre. How has this happened? And what are the implications?
Trends facing Home healthcare today
1. Costs are out of control
The U.S. now spends more on healthcare than it does on food. With skyrocketing costs along with downward pressure on revenue, providers must find internal opportunities.
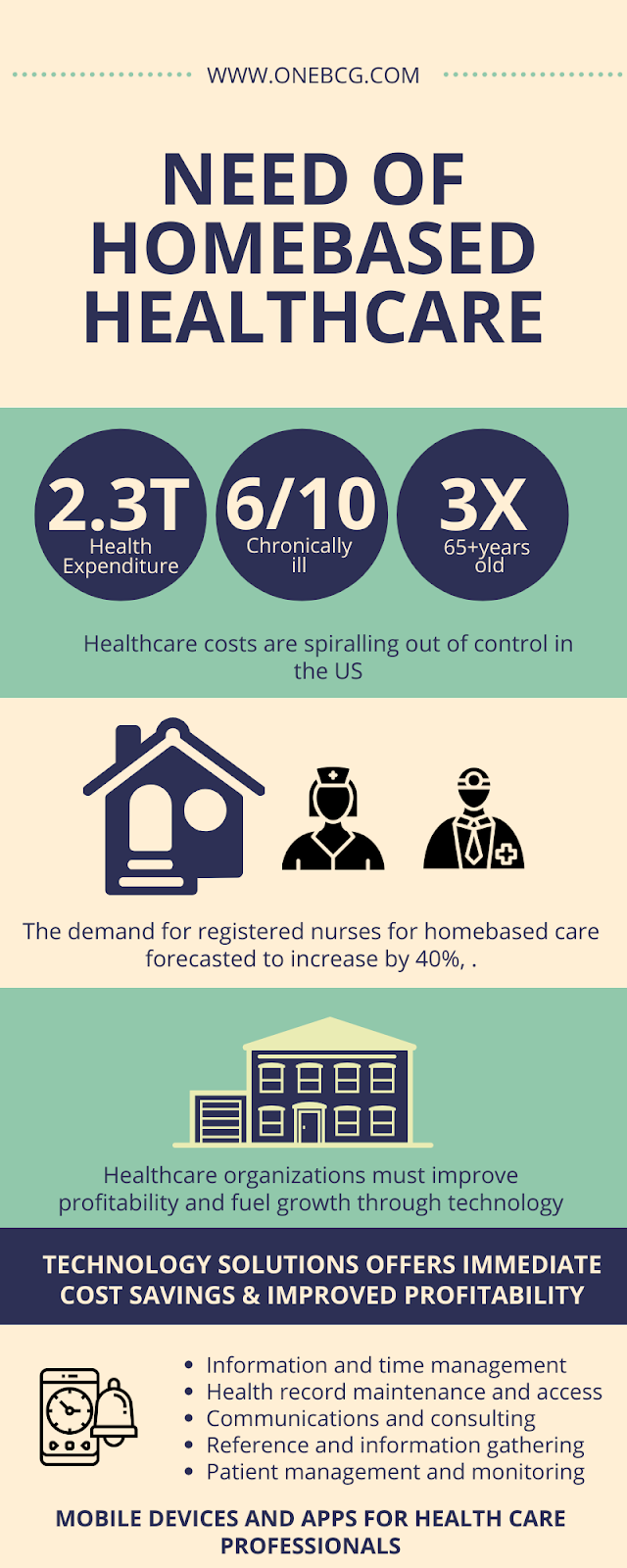
The costs associated with treating chronic conditions are enormous and burdening healthcare systems worldwide. In the United States, managing chronic diseases accounts for more than 75% of the nation’s $2.3 trillion health expenditures. About 45% of Americans suffer from one or more chronic illnesses.
2. Demand is higher than the capacity to deliver
Aging Boomers By 2030, the 65+ population is expected to triple, the healthcare use rates of the current 65+ population will double, and their spending impact is due to an increase from $1.7 trillion to $16 trillion. By 2030, more than 6 of every 10 boomers will manage more than one chronic condition.
3. Inefficiency & Quality problems
By 2020, the demand for registered nurses is forecasted to increase by 40%, while the number of nurses will have risen by just 6%.
Currently, 90% of long-term care organizations lack sufficient nurse staffing to provide even the most basic care.
Home healthcare agencies often refuse new business because of a lack of resources & capacity.
The high cost of nursing turnover adds to a reduced bottom line. The cost of filling a vacated nursing position is about 100% of a nurse’s salary.
Shortages of healthcare labour impede patient safety and quality of care efforts.
4. Productivity must increase from current assets to meet current demand, improve profitability and fuel growth through technology
Operational Efficiency offers immediate cost savings, improved profitability, and financial leverage, and this can be achieved through the right adaption of technology.
For each $1M an organization saves in operations, it can expect to enhance its capital potential by $7-9M–creating increased borrowing power for reinvestment in strategic initiatives, technologies, equipment, plant, etc.
Mobile Devices and Apps for Health Care Professionals: Uses and Benefits
Numerous apps are now available to assist Health Care Professionals with many essential tasks, such as:
- Information and time management;
- Health record maintenance and access;
- Communications and consulting;
- Reference and information gathering;
- Patient management and monitoring;
- Clinical decision-making; and medical education and training
Mobile Devices and Apps for Health Care Professionals: Uses and Benefits
Benefits Provided By Mobile Devices And Apps for Health Care Professionals:
Mobile devices and apps have provided many benefits for HCPs, allowing them to make more rapid decisions with a lower error rate, increasing the quality of data management and accessibility, and improving practice efficiency and knowledge.
Most importantly, these benefits have been shown to have a positive effect on patient care outcomes, as evidenced by a reduction in adverse events and hospital length of stay. These and other benefits mobile devices and apps provide to HCPs are discussed in the following section.
- Convenience: Health care professionals associate numerous amenities with using a mobile device in clinical practise, such as portability, rapid access to information and multimedia resources, flexible communications, and a choice of powerful apps to accomplish many different purposes.
- Better clinical decision-making: Many medical apps make mobile devices invaluable tools that support clinical decision-making at the point of care. The use of mobile devices can also help better decisions by pharmacists by providing instant access to multiple drug information sources and other medical references.
- Improved accuracy: Mobile devices have repeatedly been found to improve the completeness and accuracy of patient documentation, an effect that has often been attributed to ease of use. Based on a more detailed description of clinical findings and a correct progress assessment, documentation prepared using a mobile device was judged to be of higher quality than documentation prepared using paper records.
- Increased efficiency and enhanced productivity: The use of mobile devices has been shown to provide HCPs with numerous increased efficiencies, including improved quality of patient documentation through fewer errors and more complete records, more rapid access to new information, and improved workflow patterns. Mobile apps can also help increase Productivity by improving professional and personal time and information management.
